4 ADHD Medication Considerations during Pregnancy and Nursing

Managing medication during pregnancy and postpartum can add an extra layer of complexity to an already uncertain time
Pregnancy is a period of profound change. A common question is whether to continue or discontinue ADHD medication during pregnancy or while nursing (lactating). This decision requires balancing the potential risks of medication exposure to the challenges of managing ADHD symptoms without medication. Below we look at what the scientific literature has to tell us to date.
Stimulant versus Non-stimulant ADHD Medication
Briefly, it is important to recognize the difference between the two most common classes of medications for ADHD: stimulant versus non-stimulant medication. Stimulants refer to medication that contain a form of methylphenidate or amphetamines, such as Ritalin or Adderall. On the other hand, non-stimulant medications, such as Strattera or Intuniv (guanfacine) act on different neurotransmitters.
The latest research
Since this blog was published, there has been some exciting new research out of Denmark to suggest that ADHD medication during pregnancy is safe for mothers to take regardless of which trimester they took the medication or the type of ADHD medication. The study compared women who discontinued their ADHD medication during pregnancy to women that continued to take their ADHD medication during pregnancy to see if there were differences in effects on the baby immediately and over time. Luckily, they found no significant differences between the two groups! Please continue to consult your healthcare provider about the best option for you. EndeavorOTC offers a non-medication option to treat symptoms of ADHD that can be used with or without medication treatment.
The decision to use medication during pregnancy and postpartum is not a one-size-fits-all answer. Always consult your healthcare provider; this information aims to help support that conversation.
Here are 4 factors to consider for your ADHD treatment during pregnancy:
-
Type of medication
A recent systematic review sought to identify if ADHD medications were a teratogen during pregnancy and lactation (nursing); however the authors caution we still need more high quality studies (Li et al., 2021). There were not enough studies with high quality samples (large enough sample sizes) to understand the relationship between ADHD medication and offspring effects during lactation, but the study was able to find some themes with ADHD medication during pregnancy (Kittel-Schneider et al., 2021). There was preliminary evidence that stimulant medication has a small increased risk of preeclampsia and preterm birth compared to a non-stimulant medication (Li et al., 2021). However, more research is needed to draw conclusive statements.
-
Timing of medication use
The answer to ADHD medication use during pregnancy may also depend on the timing of medication use. The first trimester of pregnancy the fetus is most vulnerable to developmental effects. Your healthcare provider may recommend you stop medication during this period of time, but potentially resume medication in your second or third trimester (Kittel-Schneider et al., 2021).
-
Alternative strategies to medication
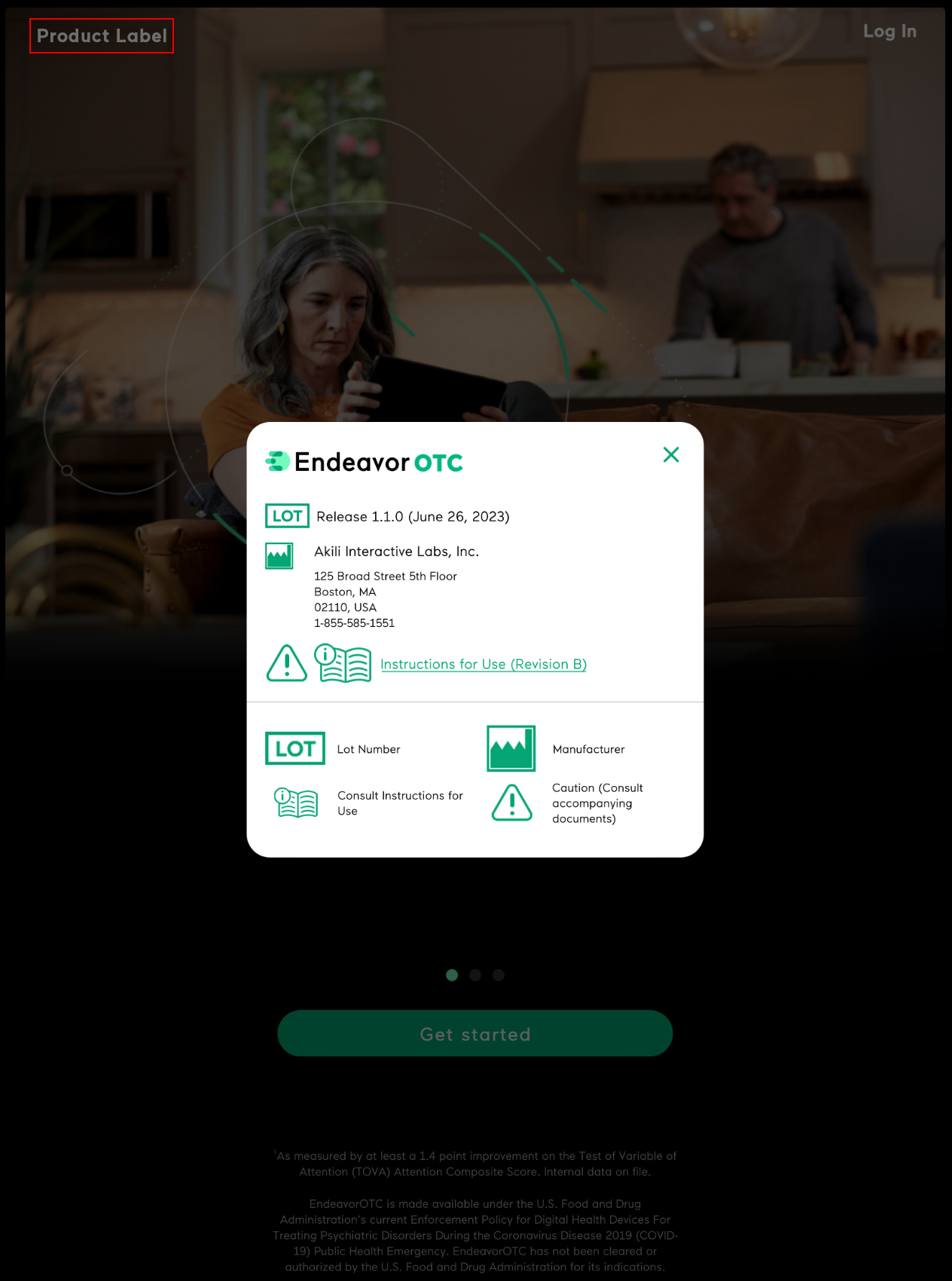
Depending on your circumstances and presentation, pregnancy may be a time to pursue non-medicated options to treat your ADHD. Evidence-based methods to medication alternatives to ADHD include cognitive behavioral therapy, lifestyle changes, or cognitive treatments for ADHD. EndeavorOTC—a non-medication treatment that is proven to reduce ADHD symptom severity and improve focus—can be a safe option for pregnant women. Please review more information on EndeavorOTC and speak with your healthcare provider to see if it might be right for you during this time. -
Symptom severity
While there are different risk factors to weigh regarding medication during pregnancy or while nursing, it is also important to consider the risk factors of non-treated ADHD. Untreated or controlled ADHD symptoms during pregnancy and postpartum could lead to increased stress, impairment in daily function, and increased risk of mental health challenges (Kittel-Schneider et al., 2021).
Seeking Professional Help
If you suspect you have ADHD or notice significant changes in your symptoms during pregnancy or postpartum, consult your healthcare provider. A professional evaluation can determine the best approach to managing ADHD while ensuring the well-being for both the mother and child. Timely intervention can contribute to a healthier, more balanced motherhood experience.
Note, while this article predominantly discusses ADHD in terms of birthing parents, it is important to note that there are both sex and gender influences on ADHD presentation. More research is needed into understanding ADHD interactions with pregnancy for birthing parents that do not identify as women.
About the Author
-
Jessica E. Flannery, PhD is the Associate Director of Clinical Science at Akili. She is a clinical licensed psychologist, an ADHD-Certified Clinical Services Provider (ADHD-CCSP), and a developmental social neuroscientist. She has published over 50 peer-reviewed articles, received prestigious fellowships and awards and is a prior TEDx speaker.