Research Roundup: The Latest Study on ADHD Medication and Pregnancy

Pregnancy and medication: a confusing landscape
A positive pregnancy test comes with a rainbow of emotions—excitement, relief, fear, and hope, to name a few. But for pregnant people using medication to manage their ADHD, a positive pregnancy test also comes with a big question: Do I have to stop taking my ADHD medication while I’m pregnant? What about when I’m nursing?
Currently, the FDA classifies ADHD medications as “pregnancy category C,” which means we don’t have sufficient information to confirm whether they are harmful or not. When I was pregnant with my daughter, I quickly learned that this “category C” designation applies to a slew of medications, some of which surprised me—including something as seemingly harmless as Tums, which I learned through a frantic Google search when third trimester heartburn kicked in.
This uncertainty and lack of data stem from the fact that it’s very hard to design a true controlled research study in pregnancy, since it would mean exposing a fetus to a medication when the risks of doing so are unknown. The solution? For these category C drugs, healthcare providers basically have to make a judgment call. They weigh the potential benefit to the pregnant person (and costs of not taking the medication) against the existing research evidence—which is often piecemeal and observational—of potential harms to the fetus.
New research evidence on ADHD medication in pregnancy
For all these reasons, I was very excited to read this new study on ADHD medication during pregnancy, which provides updated research evidence about the risks to a fetus exposed to ADHD medication. I’ll give you the take-home up front: researchers found no greater risk of any physical or mental problems in children who had been exposed to ADHD medication during pregnancy, providing reassurance for patients with ADHD who are considering continuing their ADHD medication during pregnancy.
Now let’s dig a little bit into the methods of this study, which are very important when evaluating how compelling the research is.
What’s promising about this particular study is that it was a population-based cohort study, which means that the researchers looked at data across every single birth for a specific period (here, 1998 to 2015), for the entire country of Denmark—a total of 1,092,668 babies.
This type of study is possible in a country like Denmark because the entire population has access to the same healthcare system, and they have national registers that track demographic and health data.
In this study, the researchers followed all babies born in 1998 through the end of 2018 (20 years!), or until death, leaving the country, or a diagnosed health problem, whichever came first. They compared the 898 babies exposed to ADHD medication during pregnancy (stimulants: methylphenidate, amphetamine, dexamphetamine, lisdexamphetamine; non-stimulants: modafinil, atomoxetine, clonidine) to the 1,270 babies born to mothers who had used ADHD medications before becoming pregnant but discontinued use during pregnancy.
For both groups, they looked at whether the babies developed neurodevelopmental psychiatric disorders (ADHD; autism spectrum disorder), other neurodevelopmental impairments (e.g., impaired vision or hearing; epilepsy; seizures), and growth impairments. Importantly, results showed that the group exposed to ADHD medications during pregnancy was no more likely to develop any of these conditions than the group whose mothers discontinued ADHD medication during pregnancy. While past studies had similarly shown that ADHD medications did not seem to place a fetus at any increased risk, they were in much smaller samples, which made researchers and clinicians less confident in the findings.
Implications for clinical care
So practically, what does this new study mean for people with ADHD evaluating whether to continue their medication treatment during pregnancy? Akili’s medical and scientific team recently had an internal discussion about the implications of this study for our patients (yes, we’re nerds).
We talked about how on the one hand, these results from Denmark are exciting—they could empower women with ADHD staring down at a fresh positive pregnancy test, and their doctors, to make more informed decisions. On the other hand, a neuroscientist on our team aptly pointed out that in practice, it’s unlikely that a single study like this will have much of an impact on routine clinical care, at least in the near term. She reminded us that it takes years, if not decades, and a whole lot of research for clinical guidelines to be updated—and it’s understandably easier and safer for providers to be conservative in their advice to patients during pregnancy.
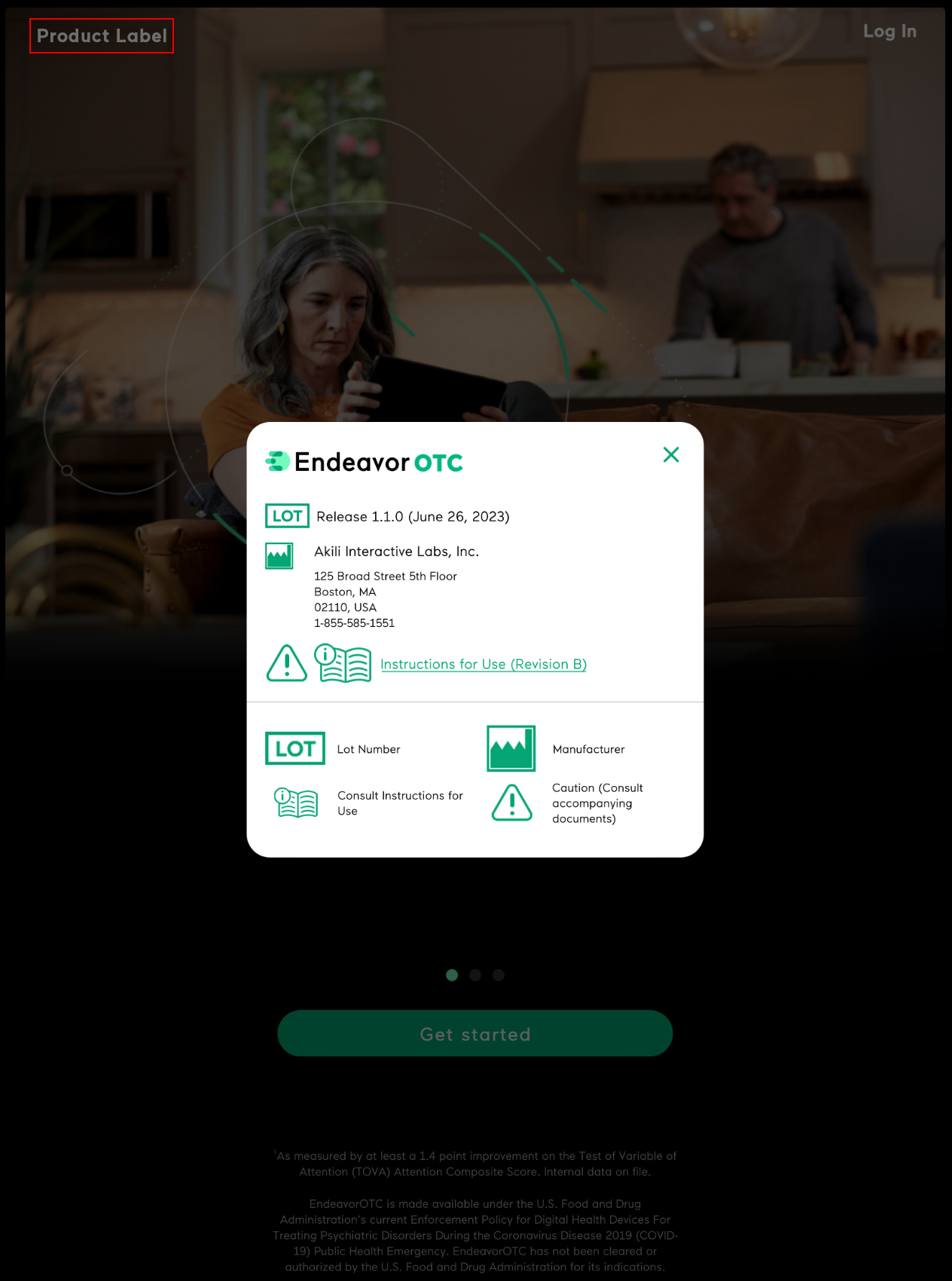
So even with promising findings like these supporting the safety of ADHD medications during pregnancy, many pregnant people and their doctors will continue to err on the side of caution, potentially choosing to discontinue ADHD medication or reduce their dose. That’s where having lots of options in your ADHD treatment toolkit is critical, and why we at Akili are so passionate about expanding access to safe, non-medication treatments like EndeavorOTC.
About the Author
-
Dr. Caitlin Stamatis, PhD, is a clinical psychologist and researcher focused on novel uses of technology for mental healthcare. Her 40+ scientific publications have been featured in leading journals such as Nature Partner Journal: Mental Health Research, Depression & Anxiety, and Emotion. Dr. Stamatis has spent her career leading clinical research and product development to build and evaluate new digital mental health treatments, at both big companies like Google and more rapidly growing, specialized digital therapeutics companies like Akili.